The arrival of a new class of drugs that curb appetite — including semaglutide, sold as Ozempic and WeGovy by the Danish company Novo Nordisk — has triggered a surge in their use to accelerate weight loss. In 2023, around 1.7% of people in the United States were prescribed a semaglutide medication, and demand is growing fast around the world.
These injectable drugs could help to prevent and treat diabetes and other chronic conditions often associated with obesity — classed as having a body mass index (BMI; weight divided by height squared) of more than 30. The World Obesity Federation in London estimated that 770 million adults worldwide could be classed medically as obese in 2020, and predicts that the number could exceed one billion by 2030.
Weight loss, however, is not just a medical phenomenon — it’s a social one, too. As anthropologists, we’re well aware that drastic weight loss can reshape people’s social lives and emotional well-being in negative as well as positive ways.
Four key questions on the new wave of anti-obesity drugs
We’ve seen it before, in the context of weight-loss surgery. Between 2013 and 2016, through in-depth interviews, we traced the journeys of 35 people undergoing bariatric surgery in the United States. We tracked the experiences of another 300 individuals through surveys1. Bariatric surgery restricts food intake and absorption by reducing the size of the stomach and, often, the length of the intestine. The people we worked with experienced greater self-confidence, in addition to health benefits, after their surgery. But many also had to cope with both unpleasant physical side effects and harsh judgements from others about their choice to lose weight through surgery, rather than through diet and exercise.
We anticipate that people who take drugs to lose weight will be similarly affected by side effects and judged by others, with consequences for well-being and mental health. Many people who qualify for the drugs on prescription because they have a BMI of more than 30 will have no weight-associated health complications — unlike those who undergo bariatric surgery in an accredited programme, who typically have at least one chronic health condition. Moreover, with the drugs increasingly sold off-prescription or on the black market, people with BMIs of less than 30 will try them, too, and might experience unnecessary adverse consequences.
Here, we call for an urgent and realistic discussion about the social downsides of achieving substantial weight loss through drug use, informed by experiences around bariatric surgery.
Weight is a social issue
Humans excel at judging one another. Bodies — weight, height, clothing, physical signs of disease — are often central to these assessments, in part because they are so visible. In a world of increasingly sedentary work and processed food, ‘thinness’ is difficult to maintain. And so, around the globe, slimmer bodies have become associated with a higher social status2.
Thinness is also widely linked to good health in popular culture, even though science suggests a more complex picture. Although a high BMI has been linked to diabetes, for example, it is also a predictor of lower risk of stroke3. In 2023, the American Medical Association in Chicago, Illinois, acknowledged that BMI should not be used as a sole measure for assessing health (see go.nature.com/484j2dt).

The idea that weight loss should be achieved through exercise is rife in popular culture.Credit: Matt Sayles/AP Images for Weight Watchers/Alamy
At the same time, stigmas abound around ‘fatness’4. Compared with people who are clinically defined as at a ‘healthy’ weight, those defined as obese report being treated by health-care providers with less care and compassion, having less choice of romantic partners and less access to educational and career-advancement opportunities5. Women seem to be particularly at risk of such discrimination2. For example, heavier-weight daughters tend to receive less financial support for university from their parents than do lighter-weight female students from families in similar financial circumstances6.
There is also a widespread sociocultural myth that becoming and staying thin should be achieved through arduous and morally valued dietary control and exercise. Being fat is seen as a sign of laziness and of a lack of self-discipline — but so is the use of medical interventions to help lose weight7. Social-media posts provide myriad examples of how weight loss and staying slim through diet and exercise is viewed as a virtuous achievement. This general idea that success should be the outcome of personal effort is embedded in many aspects of contemporary life, including education and wealth8.
Judged for weight loss
Such cultural beliefs profoundly influenced the weight-loss experiences of the people with whom we spoke1.
How stigma subverts public health
More than half of our US study participants didn’t tell people other than close family that they were undergoing bariatric surgery, because they feared judgement. This fear was borne out in the remainder of the cohort — among those who did speak openly about their surgery, 90% were told by at least one person in their social networks that they were cheating at weight loss. Because they underwent a surgical intervention, they were viewed as not working hard enough, not showing enough discipline or not displaying enough moral fortitude to ‘deserve’ their weight loss. They had lost their physical weight, but they still carried the stigma of being labelled as lazy and undisciplined.
We found the same pattern in Brazil, where women who underwent bariatric surgery were told by family, friends and strangers that they ‘took the easy way out’9.
Such judgement has a cascade of emotional and behavioural effects. Women in Brazil reported a range of reactions to being judged, from anger and frustration to resigned acceptance and agreement. Stress around body weight was a common response in our US interviewees. Stress, in turn, can affect digestion, the immune system, cognitive function, emotional regulation and more — particularly unwelcome at a time when the body is undergoing profound physical changes from surgery. Interviewees worried that their eating would become uncontrolled, and that they would ‘stress eat’ in adverse situations, including when they felt judged10. Sixty-four per cent of our survey respondents reported that they were only ‘somewhat adherent’ to the strict diet required after surgery, and that this self-perceived failure increased their stress, creating a vicious cycle of negative emotions that can make dietary control even harder.

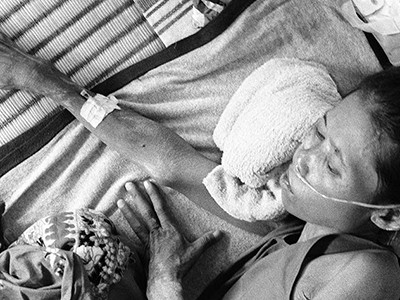
Bariatric surgery should not be considered an easy route to weight loss.Credit: Kathy Young/AP/Alamy
And because many people hide the fact that they have had surgery, open discussion about their experiences is lacking in the public domain. Our interviewees often cited reality television as their main source of knowledge about bariatric surgery before coming to the clinic. In such TV programmes, surgery and the resulting weight loss are often portrayed as the successful end point, with ongoing challenges over the following decades mostly invisible.
In real life, managing extreme weight loss is a life-long effort. Thirty-six per cent of our survey respondents reported chronic struggles with vitamin deficiencies, and 47% reported new food intolerances after surgery. Nausea was common — as it is for those who take anti-obesity drugs. Other side effects of rapid, extreme weight loss — by any means — include a drawn face and loose, sagging skin that can be painful and becomes infected easily1. As well as being physically challenging, such bodily features are viewed societally as unattractive.
In our view, the widespread enthusiasm for weight-loss drugs is not just a solution to a medical problem — it’s also a response to deeply held, widespread fear and anxiety around body weight. The stigma of being labelled by others as fat can shape decisions to use weight-loss medications, and with weight loss comes the expectation of a ‘better’ life with more social acceptance. But, as our research with people undergoing bariatric surgery shows, weight-loss trajectories are not that simple. It’s crucial that pharmaceutical companies, clinicians and researchers consider the emotional aspect of decision-making around anti-obesity drugs.
Next steps
First, pharmaceutical companies should market drugs in ways that avoid promoting weight loss as an easy fix. The physical side effects of rapid weight loss should be made clear.
The sting of sizeism in the scientific workplace
Next, as part of this effort, drug firms and researchers should focus on understanding and communicating the interconnected emotional and social ramifications of rapid weight loss. Gaining this knowledge will require tracking the experiences of people using Ozempic, WeGovy and similar drugs over years — by following their changing health, trajectories of weight loss and gain, and their attitudes towards and understanding of these changes. This research must account for the fact that a person’s emotional well-being is dependent on context, by examining how the attitudes of social circles and broader society affect each individual’s experience.
Finally, clinics and physicians should support people who are taking weight-loss drugs. Our bariatric-surgery cohort highlighted the clinic’s support programme as one of the biggest factors in post-operative satisfaction. Educational seminars before surgery enabled participants to make an informed decision about whether the benefits of surgery outweighed the costs for them. Individuals could also access a support group after surgery, to discuss issues and receive support and affirmation. Without this programme, our interviewees told us, they would have had a much harder time coping with negative feedback and judgement.
Similar resources should be provided for those who are prescribed weight-loss drugs. These resources don’t need to be in-person — quality educational programmes can be provided online. But they do need accredited professionals and trained moderators, to prevent the risk that participants without medical background will share health ‘tips’ and information that are not medically sound.
Taking such steps to ensure that people understand the physical and emotional pros and cons of weight-loss drugs is crucial, to prevent a cascade of unexpected negative social and emotional effects among the millions of people who will take anti-obesity drugs in the coming years.
Source link